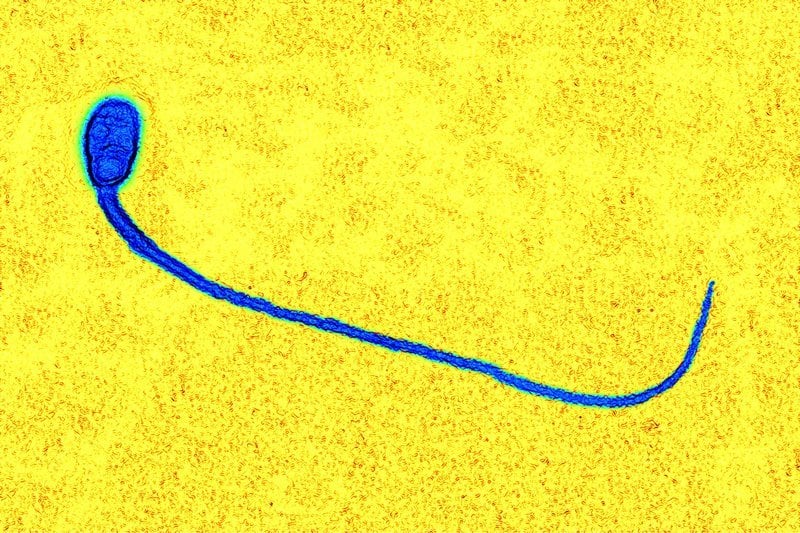
Researchers from Cambridge University’s Gurdon Institute have made significant progress towards the replication of human sperm cells in the lab. Their work, which employed miniature artificial testicles to support cell development, is a vast improvement on past endeavors.
In fact, the breakthrough is a significant milestone, a “halfway point” in the development of viable artificial sperm cells, with some suggesting that one day the technology could be used in the treatment of male infertility.

Stepping It Up from Mice to Men
The natural production of sperm in the body is complicated to say the least; and while researchers have made claims about successful attempts to reproduce the process in the lab, these attempts were quite far from the real thing.
For example, in one study, researchers were able to produce mouse offspring from eggs fertilized with artificial spermatids. However, some have been critical of these findings, citing that the results have been hard to replicate. Furthermore, spermatids are immature sperm cells that cannot swim, not complete viable sperm. As such, they need to be manually introduced into the eggs for fertilization to occur.
Then there’s the fact that much of the research aimed at creating sperm cells and using them to produce viable offspring have involved mice. Stepping it up to human reproduction is a giant leap ethically, but also scientifically.
“The challenge is that the timelines are very long in humans,” Azim Surani, of the University of Cambridge’s Gurdon Institute said when speaking with the Guardian. Early human cells follow the same developmental pathway until about the eight-week mark, where they diverge and become either sperm or egg cells. In mice, this divergence happens after 13 days. The lengthy developmental time frame in human cells has proved to be a real stumbling block.

Artificial Testicles the Key to Recent Success
In previous research, Surani and his team reached the four-week mark using human cells; still four weeks short of the point at which cells become either sperm or eggs. However, the team wanted to reach the critical eight-week mark in their latest efforts.
To that end, they developed artificial testicles, or gonadal organoids, to provide the right biochemical cues, or timing, to impel the cells towards further stages of development. These artificial testicles were essentially blobs of gonadal cells in gel, and despite this formulation seeming somewhat elementary, they did indeed provide the right environment for improved cell development.

Towards a Cure for Infertility
Replicating the intricacies of sex cell development, and getting it right, is extremely challenging and complex. Surani acknowledged, “If this was ever going to be used in a clinical setting we have to be sure that it has gone through all the right stages – all of these steps are incredibly important… You can make an egg that looks like an egg, but it might not be the right cell in molecular detail. You could get a lot of problems with that. You don’t want something that’s going to grow into some kind of abnormal structure.”
However, the research offers some hope to couples unable to conceive naturally; moving towards a better understanding of infertility and its causes. And while the use of artificial sperm and eggs is banned in some countries, if scientists could perfect the technique, regulators may re-examine the rules.
Either way, the research is a big step forward in our understanding the delicate and precise mechanisms associated with human reproduction. Speaking to the Guardian, UCL director of reproductive science and women’s health Helen O’Neill said, “Much of the ambition to recreate reproductive processes in the lab is to further our understanding of these processes… It is surprising how little we understand about the fundamental dynamics of the beginnings of life.”